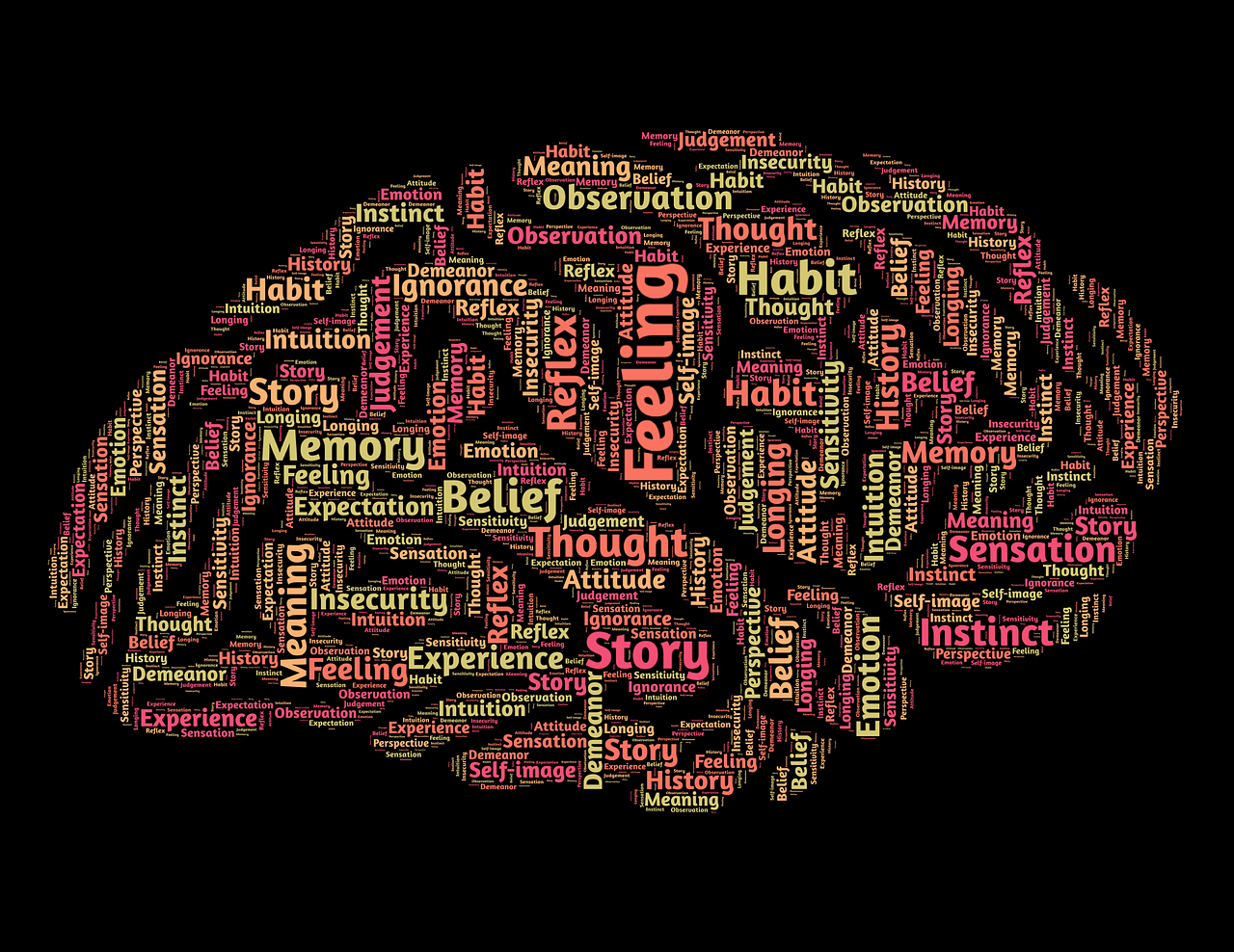
If we didn’t have habits, life would be really difficult. All of us have developed patterns of moving, thinking, and behaving that become deeply ingrained in our nervous systems, like well-carved out ski slopes during peak season. These patterns are represented in our brains as neural networks, or interconnected brain cells that fire together to create our ways of being. The brain creates these networks to ensure efficiency. Without these networks, we would have to start from scratch every single day with clean slates, no skills, and no purposeful movements available to us, like a newborn baby.
As we go through our development, we learn a heck of a lot. In fact, by the time we are adults, our 100 billion neurons can form over 100 trillion synaptic connections! We continue to learn as we grow older, although our brain does go through certain critical periods, making it more or less responsive to learning certain types of information throughout various parts of our lives. This is why it is so much easier to learn a new language as a child, as early childhood is the critical period for language development. Our youth is also a time where we develop many of the neurological patterns that define who we are, what we do, and how we think.
When it comes to movement, our repertoire tends to shrink as we grow older, and we are more likely to move in a less variable, more confined way, which gives rise to challenges with mobility in our later years. We are more likely to fall back on the same patterns again and again, and less likely to expand our horizons.
While the learning process is extremely adaptive and helpful for our ability to engage in life, our learning can also lead to undesirable habits and patterns. For example, imagine that you grew up in the north with a very questionable heating system. Whenever winter would come along, you might bundle up in a few coats, and find yourself shivering and hiking your shoulders up towards your ears more often than you might like.
The more time you spend generating tension in your shoulders, the more of a habit it might become. So later on, even if you move down south, you might have the learned habit of tensing up the shoulders, particularly during times of increased stress. This can impede the natural movement and flow of your body, and might contribute to strain on the tissues and chronic discomfort.
We all have our bodily habits. Whether it’s hiking up the shoulders, clenching the jaw, craning our necks forward during computer work, tensing the pelvic floor, holding our breath during exercise, only crossing the same leg on top while sitting, or countless others. What these habits have in common are that they are learned, persistent, and undesirable- and, they may have served us some helpful purpose in the past. That’s why they exist.
Sometimes we don’t even notice these habits until someone else points them out- a family member, a friend, a physical therapist. Sometimes the habit is completely innocuous and may or may not be associated with something undesirable. If in fact the habit is truly undesirable, e.g. it relates to unwanted strain on a tissue, is associated with discomfort, etc., then we are likely trying to change the habit. How do we do this?
Building Awareness
The first step of creating change is awareness. If you do the habitual behavior 100 times per day, and only notice it one time, this is not enough. Performing mind-body practices regularly such as Feldenkrais lessons, yoga, tai-chi, mindfulness meditation, etc. will help to develop the ability to become more aware.
In everyday life, a reminder system must be developed. One must become aware of the situations and environments in which the undesired habit is most likely. Does the habit show up the most frequently at the computer? While driving? In the kitchen? Wherever the habit is likely to show up, consider bringing a visual cue into the area, such as a brightly colored sticky note. The sticky note could be blank, have a small symbol to remind you to cease the habit, or a few words or short phrase, such as “exhale”, “relax your shoulders”, “smile”, etc.
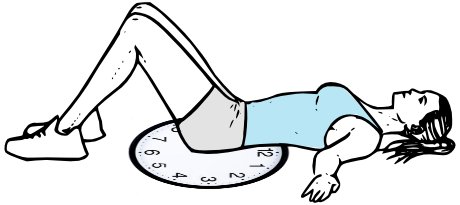
During the activities that are most likely to trigger the habit, consider a very short body scan, perhaps right before starting the activity, sometime during, and immediately after. Say that you are going to do desk work for one hour. Right before you begin, sit down, get comfortable. Close your eyes. Ask yourself if you are comfortable. Ensure that your breathing is nice and relaxed. Scan your attention throughout your whole body, particularly the area where the habit might show up. Maybe this takes 15-30 seconds. Continue on with your task, but do the same thing half way through, and again after finishing the task.
Respond with Kindness
When you inevitably notice that the habit is happening, change how you respond to it. It is very easy to become frustrated with yourself- “What’s wrong with you, why can’t you stop doing that!”. This is an unhelpful strategy, as it creates unnecessary frustration and suffering around the habit. Instead, have a chuckle. “There you go, tensing your shoulders again like it’s freezing! No need- you are safe and comfortable.” This is making friends with your habit. Your habit is there for a reason, and by being kind to yourself, you are more likely to develop a better relationship with it.
Purposefully Move the Involved Tissues
And finally, when you notice the habit arising, perform some movement that helps to relax and change the tension in the area. For example, if the habit is hiking your shoulders up, here is a movement sequence you can try. Start by raising and lowering both shoulders, towards and away from your ears, as if your shoulders are two rising elevators. Then, let one shoulder shrug up as the other goes down, like two elevators going in opposite directions. Finally, begin to circle both shoulders up, back, down and around. This can become both shoulders making circles, but at opposite phases of the circle, so as one shoulder is up the other is down (like two ferris wheels going side by side). Perhaps you spend no more than a minute on these movements, and then return to whatever task you were engaging in.
By implementing these you will begin to create more instances of noticing the habit, and changing how you respond to it to be that of kindness, as well as an active movement-based strategy to change how your nervous system communicates with the involved muscles.
These strategies can greatly decrease the frequency and impact of the habit, and can facilitate the creation of new habits! The nervous system will begin to choose less stressful and more efficient movement patterns, which can eventually replace or minimize the influence of long-term, inefficient movement patterns. Over time, the new patterns can become automatic. While the old habits may never disappear completely, you will find it comes up less often, you will notice when it happens more often, and it will lead to overall less distress and discomfort.
Written by Jacob Tyson, DPT - Physical Therapist, Yoga Instructor and The Wellness Station Team
Images:
https://online-learning-college.com/wp-content/uploads/2022/04/Neurons-and-synapses-scaled.jpg
https://protailored.com/wp-content/uploads/2021/11/AdobeStock_113929106-scaled-1.jpeg
https://encrypted-tbn0.gstatic.com/images?q=tbn:ANd9GcQtb4YBvroHNzQwP9I32MnaJpXJfhTsYqUHes8j2IaFLA&s
https://d5sbbf6usl3xq.cloudfront.net/alternate_shoulder_shrugs_close_up___yoga.png
https://domf5oio6qrcr.cloudfront.net/medialibrary/10054/GettyImages-1151196088.jpg